Institutional News
Dr. Nan Tang’s laboratory revealed that the adult AT1 cell population consists of two distinct subtypes that differ in cell fate.
On February 20, 2018, Dr. Nan Tang’s laboratory published a paper entitled “The pulmonary alveolar type I cell population consists of two distinct subtypes that differ in cell fate” in PNAS. In this study, they discovered and demonstrated the heterogeneity of AT1 cells during alveolar development and regeneration.
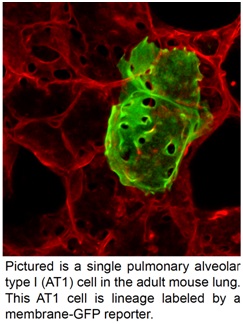 Pulmonary alveolar type I (AT1) cells
cover more than 95% of alveolar surface and are essential for the air-blood
barrier function of lungs. Very little is known about the molecular genetics
and fate specification of AT1 cells.
Pulmonary alveolar type I (AT1) cells
cover more than 95% of alveolar surface and are essential for the air-blood
barrier function of lungs. Very little is known about the molecular genetics
and fate specification of AT1 cells.
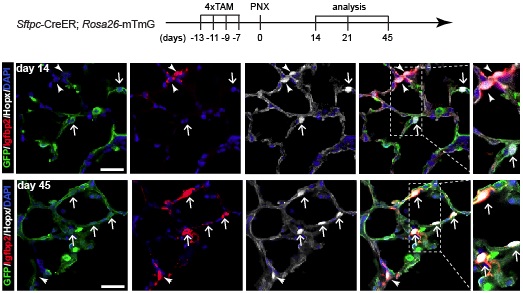
AT1 cells were traditionally considered to be terminally differentiated cells. However, a recent study found that adult AT1 cells retain cellular plasticity and are able to proliferate and to give rise to AT2 cells during post-peumonectomy(PNX) alveolar regeneration.Owing to the lack of knowledge of the development and heterogeneity of adult AT1 cell population, it is unclear whether all or only a subset of AT1 cells can trans-differentiate into AT2 cells during alveolar development and/or alveolar regeneration. Additionally, the development and differentiation of AT1 cells during alveologenesis and alveolar regenerationarestill poorly understood owing to the difficulty of isolating these fragile cells.The researchers applied a combination of single-cell RNA-seq analysis, mouse genetics, and an alveolar-like organoidculture systemand characterized AT1 cell development during both postnatal lung development and alveolar regeneration. They identified a novel genetic marker of postnatal AT1 cells, insulin-like growth factor-binding protein 2 (Igfbp2), and use this marker to demonstrate that the postnatal AT1 cell population contains two unevenly distributed AT1 cell subtypes, Igfbp2+Hopx+ and Igfbp2-Hopx+ AT1 cells. Igfbp2 is heterogeneously expressed in AT1 cells of newborn lungs and newly differentiated AT1 cells (from AT2 cells) that occur during post-PNX alveolar regeneration. The proportion of AT1 cells that express Igfbp2 increases during normal alveologenesis and during post-PNX formation of new alveoli. Importantly, they demonstrate that Igfbp2+Hopx+ AT1 cells represent the terminally differentiated population of AT1 cellsand do not trans-differentiate into AT2 cells in normal or post-injury lungs. This study found that some of the newly differentiated Hopx+Igfbp2- AT1 cells likely to maintain developmental plasticity in the period before these cells begin to express Igfbp2—these Hopx+Igfbp2- cells can trans-differentiate into AT2 cells and thus help maintain tissue integrity in the context of repair during injury-induced alveolar regeneration.
More and more evidence is suggesting that adult AT1 cells have a variety of other functions beyond their known roles in the formation of the air-blood barrier and in transporting ions and water. This study provides tools and insights that will guide future investigations into the molecular and cellular mechanism(s) underlying AT1 cell fate specification during lung development, regeneration and diseases.



